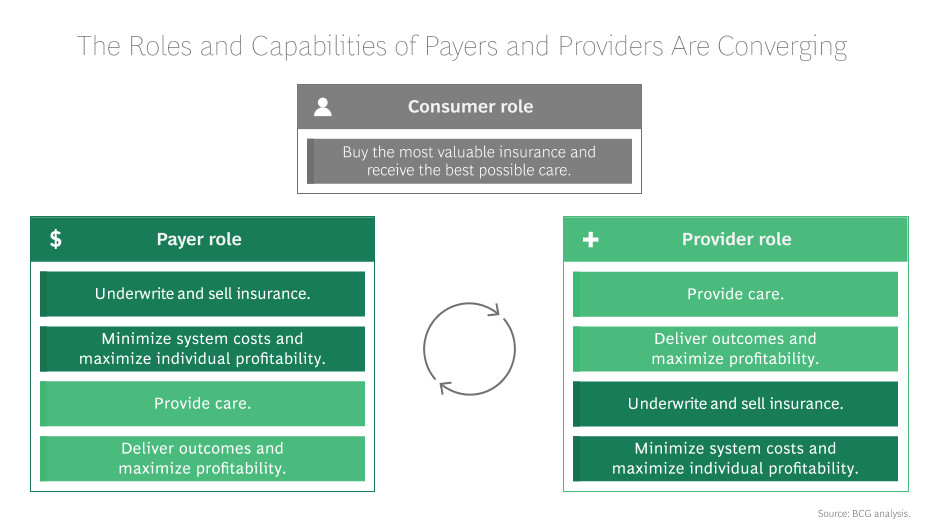
When payers and providers don’t collaborate, the patient needs to take the extra initiative and burden of forcing the communication between both sides—dealing with multiple bills, different opinions on their outcomes and, sometimes in extreme cases, dealing with hidden costs payers or providers were unaware of. This is unacceptable. As time goes on, payers and providers must be united. Once aligned, this hybrid of information will lead to better health outcomes, an enhanced care mode and clear financial wins for both sides. A clear, collaborative model must be adopted for the two sides to join together to deliver a better patient experience.
According to Andrew Underhill, a chief technologist at Systems Made Simple:
GET A PERSONALIZED DEMO
See for yourself what best-of-breed employee engagement software can do for your company
We’ll show you how Jive can unite your organization and bring out the best in your workforce.
Schedule A Demo
Frequently Asked Questions
We’ve got your back every step of the way!
Here are 4 top tips to build employee engagement in your workplace:
- Create a positive work environment.
- Encourage employees to collaborate and connect.
- Use an employee intranet portal to increase internal communication.
- Encourage open communication.
There are many employee engagement tools available. Jive offers an industry-leading intranet platform that empowers employees and increases engagement.
Here are 3 easy ways to measure employee engagement:
- Conduct an employee survey.
- Use HR employee engagement software.
- Introduce an incentive-based strategy.
An engaged employee is a productive employee. The more engaged an employee is, the lower the turnover rate will be for your company.
Employee engagement has a direct impact on lowering employee turnover rates. HR leaders should focus on increasing engagement in order to shore up employee retention and boost productivity.
Answer these questions to know if your employees and managers are highly engaged:
- Are your employees and managers absolutely clear about the company’s core values and goals?
- Do they actively communicate and collaborate on your company intranet platform?
- Can they see how their contributions are adding value to the company’s success?
- Do the managers have good leadership skills?
- Do employees have access to all necessary tools?
- Are employees happy and motivated to work?
An HR employee engagement platform in an employee engagement solution that helps organizations increase job satisfaction and improve employee retention.
Most engagement strategies lack a sense of employee empowerment. When employees feel powerless, they lack confidence in the organization, and their involvement decreases with time. At Jive, we offer an interactive intranet platform that empowers employees to communicate, share files and get work done. With Jive, employees feel empowered, connected, and most importantly- engaged with their work.
In an organization, “engagement” is an employee’s emotional commitment to the company and its goals. Without engaged employees, organizations can never be successful. At Jive, we offer powerful collaboration software to help employees connect, collaborate, engage quickly and help businesses achieve peak productivity.
Yes. At Jive, employees can create groups easily in our employee social network. This helps everyone connect, collaborate and share content with specific people and get responses immediately. Using groups is convenient, collaborative and cost-effective.